I will reply to this, but probably won’t be able to do it until Friday! Sorry!
Hi Eamon –
I am getting back to you from Wednesday regarding a post I made in your group and your interest in “how you perceive an authoritarian leftist influence or, politically-driven influence in the psychology fields. How does this manifest itself? & How can we articulate these interferences in the standards of care?”
Since I don’t know what your experience is in the mental health field, I am going to err on the side of providing more information about my experiences and observations, so this may end up a bit lengthy!
As I thought about your questions, there were a lot of examples that came to mind about this topic and, as you’ll see, they are wide ranging from the macro level of the field of psychology to the micro level of my own personal experiences. So you have some context of my background, I have been practicing as a clinical psychologist in Wisconsin for almost 35 years, I maintained a certification as an eating disorders specialist for 22 years and received a post-doctoral Master’s degree in Clinical Psychopharmacology in 2011. Early in my career I directed hospital programs for eating disorders but the majority of my career I have practiced on an outpatient basis and have owned an outpatient practice for 26 years.
Here are examples in reference to your questions, most of which have occurred in the past five years:
-
I have taught classes in a doctoral level graduate program. The learning objectives for each class now have to include how DEI will be integrated into the course material regardless of tthe subject matter.
-
I have also taught seminars and workshops at the post-doctoral level for practicing psychologists. All continuing education now requires sessions to include DEI in the content. The theme of the Wisconsin Psychological Association’s 2025 annual convention is “Psychology and Health Equity: Addressing Disparities and Improving Access for All” and this is one of the requirements to include in proposal submissions: “A brief statement on how your session specifically incorporates DEI.” Presentations have to align with the theme.
So, even though DEI is not my worldview and even though my practice has not been located in an area that draws a multicultural population, if I wanted to continue teaching, I would have to integrate DEI information that is outside of my scope of practice. While I have chosen not to teach anymore because of this politically driven ideology, it essentially eliminates any other points of view from the education of students and practicing clinicians. It also eliminates being able to teach or present a topic free from any political bias.
-
The vast majority of clinicians and leaders in the mental health field are liberal, so they fully support and buy in to the inclusion of the liberal agenda in all aspects of the profession. As a result, there is no tolerance for diverse opinions that are not in line with liberal ideology. A profession that is trained to accept individual differences has become fully incapable of doing so.
-
I attended a keynote presentation at a convention where the speaker was teaching on the topic of transgenderism. This was prior to 2020 when transgenderism was starting to become more mainstream. The audience was primarily composed of psychologists who did not treat transgendered patients. The education we received was that if a patient says they are transgender, we should accept that at face value and not question it because that would not be affirming their identity.
After the presentation, I spoke to the presenter and asked why as a psychologist I wouldn’t do an assessment to help determine whether the patient was actually transgender or was possibly experiencing gender confusion. I used the analogy that I have been told many times by 80 pound anorexic patients that they are completely fine and there’s no need to gain weight, yet if I just took their opinion at face value, their psychopathology would result in death. The presenter summarily dismissed me as eating disorders having nothing to do with transgenderism. He didn’t answer my question about doing an assessment, even though that is one of the core skills of psychologists.
-
I attended a continuing ed workshop where the presenter was conversantly going to use the term “trump” as in ‘this would trump that’ and physically balked after starting to pronounce “tr,” caught herself and used a different word. The topic was on self-care for psychologists, there was nothing political about her presentation, but she couldn’t use the term “trump.”
-
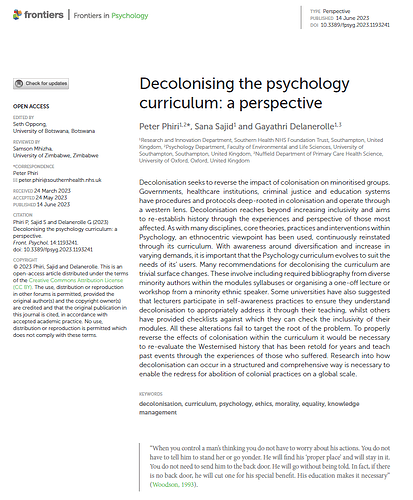
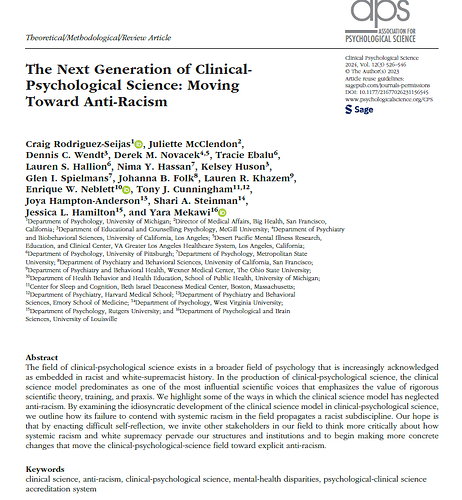
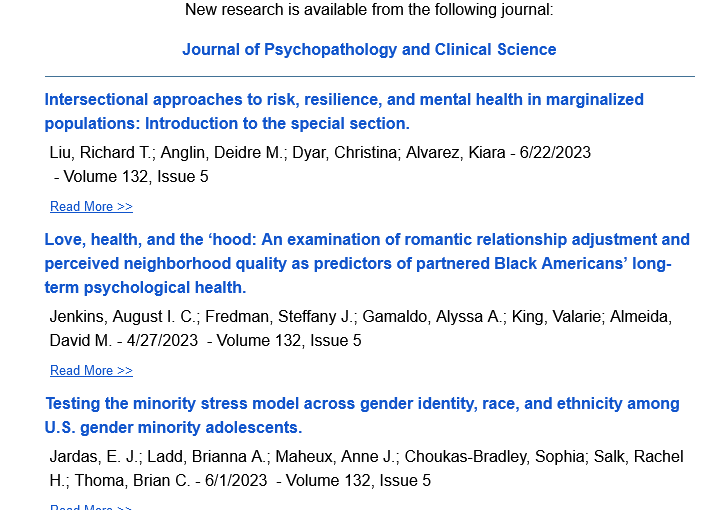
The professional literature has become infused with gender and DEI ideology. It’s hard to find a case study that doesn’t include something like “the patient is a 34 year old binary Hispanic…” The American Psychological Association has always been a liberal organization, so they drive a lot of the focus on topics like climate change, combating misinformation, immigration, election stress, gun violence, etc., within the profession.
-
I served two terms as president of the Wisconsin Psychological Association and the bylaws are clear that as a non-profit the organization’s mission is to carry out activities that support the advancement of psychology for professionals and the community. In 2020 during my past-president term, the George Floyd riots occurred and the new board of directors felt compelled to publish position statements supporting Black Lives Matter. They felt it was the duty of the board to support BLM despite the Executive Director and I explaining that the bylaws do not include political activism and, although it was their responsibility to protect WPA’s 501(c)(3) status, they were putting it at risk.
When I pointed out that the board represents the entire association membership, not just those that support liberal causes and that we needed to consider all points of view,
I was told by the Director of Diversity and Inclusion that it was “okay to discriminate against people like you (Republican) in order to not discriminate against minority populations.” I submitted my letter of resignation the next day.
-
I was aware of a continuing education seminar on the topic of how therapists should respond to patients when ‘patients commit microaggressions’ against them. An example would be if a patient didn’t know the therapist was gay and made an off hand comment about gay people. When I was trained, this would not be something that we would personalize, rather if it was clinically appropriate, we could explore where the patient developed their beliefs, whether those types of comments have ever offended anyone, etc. Now the training for an example like this is along the lines of informing the patient about the therapist’s sexual orientation and how the therapist feels about it.
-
For 30 years in the field of eating disorders a person’s normal weight was always based on genetics and not judged. In a continuing ed seminar I attended on body image, having a normal weight that is considered thin is now a “thin privilege.” Because of this, thin therapists should basically assume that this has a negative impact on patients with larger bodies and that it probably interferes with the therapeutic relationship. This seminar was taught by early career psychologists who were most likely cooked in the liberal education soup their entire lives for whom normal things become “privileges.”
-
And just for fun – I have a gay colleague who was very proud of the gay pride flag she had hanging in her office with, of course, no awareness of how this might affect non-gay patients. Can you just imagine what she would say if I had a Trump flag hanging in my office?! No tolerance for that!
Sooooo…I am one person and these are the kinds of experiences I have had! It makes it pretty clear that the authoritarian leftist, politically driven influences manifest in the education of mental health professionals and then directly impacts the care patients receive. This is why I posted that DEI and wokism need to be removed from the education of therapists and psychologists. I believe we need to return to treating psychiatric problems based on psychological theory and real, not fabricated, science.
Because of the radical shift to the left within my profession, I have dropped all of my association memberships, my eating disorders certification and, although it’s not the only reason, it has definitely contributed to my decision to retire. I don’t even recognize my profession anymore.
If you have any questions or feedback, feel free to reply! I will continue following the MAHA for Mental Health Bill thread. If there are suggestions you have for helping with the development of the bill, please let me know!
Sincerely,
Laura Lees
@Laura_Lees Thank you so so much for taking the time to draft this response. Your dedication to these issues inspires me and will do to others, to keep working and keep fighting for this.
I will read and contemplate this and get back to you asap. ![]()
For now please know how grateful I am for the participation.
Actually there is something you can help me with ![]() , I need help to identify what would be the best “Tags” to attach to this Bill. The Tags I’m referring to are the ones the site has added to the side-bar menu.
, I need help to identify what would be the best “Tags” to attach to this Bill. The Tags I’m referring to are the ones the site has added to the side-bar menu.
I need some tips on the in-roads to the government agencies, that you might be hip-to, and which, if any, of those Tags are applicable to this group. Much appreciated, and please, take care. ![]()
From A Discussion: on “institutionalized” Meditation … Good or Bad?
HI Eamon,
I don’t know how the process works regarding how the Bill will be written, submitted or who will author it, so it would be helpful to have more information about. I also don’t understand how the tags work! Is there going to be one mental health bill with a variety of topics or a variety of mental health bills written on specific topics? I haven’t found any information on the P4P website that explains how the overall process of people submitting ideas is intended to become a bill, so I’m missing the big picture!
Something to consider is that medicine by design has been siloed into subspecialties for each body system and no one looks at the entire person anymore (other than alternative and complementary practitioners). If a patient has high blood pressure, psoriasis, GERD, back pain and depression, the patient is seeing 5 doctors who rarely if ever collaborate. If we’re looking to improve the future of mental health, I think we need to drive holistic approaches that look at how the entire body is functioning synergistically and not continue the silo approach of physical health vs mental health.
In terms of in-roads to government agencies, I think we need to see how the recent Loper Bright Enterprises v Raimondo US Supreme Court decision that overturned the Chevron doctrine is going to affect government agencies. It could potentially gut many agencies and require legislative bills to be written with much more specificity. These changes won’t take place until after the election.
Laura
I love this! There seems to be no initiatives to improve mental health in our nation and if there are they are few. I am convinced mental health is the silent pandemic. We have to do better as a country.
Politicization of Human Services, & other case-studies (multimedia)
note - For vs. Against are not labeled, this is a growing topic, still compiling
I was a part of a conversation today about Emergency Room’s inability to address the mental health crisis leading to long term boarding of psych patients in EDs. They shared that 40% of individual’s first contact with mental health services is via the ER. There is a grant funded ‘pilot’ mental health ER/ walk in center in our area that can address someone’s needs in 72 minutes from walking in to walking out, including scheduling with a follow up outpatient visit within 7 days. There has been great success with the model, however, it is considered ‘not sustainable’ long term because of the lack of insurance reimbursement and the low rates for MH emergencies. They also shared that Medicaid covers the visits 100%, but commercial insurance will contribute $6 TOTAL towards the claim.
Really interesting. Thank you! @ewilson
You raise many important areas. You touch on the
- Insurance-coverage and costs problem
- The Pedestrian-Accessibility (Emergency) problem
Sorry, what’s “EDs” ? You mean ERs?
Do you happen to have a link/resource to the 'Grant-funded pilot Psych ER"?
This sounds like a good program.
Visiting a Psych Ward, is something even a very distressed and manic person will try to convince themselves is not necessary. It is intimidating and could be expensive, I don’t believe hospitals are forthcoming
with their costs.
Many people do not have insurance and are forced to make a very uncomfortable decision of denying themselves any help that might
desperately deserve. This is a failure. We really do need new model for this Emergency Care.
I’m a psychologist in private practice who graduated with my PhD in Clinical Psychology in 1993. I’ve also worked in various other settings, such as inpatient hospitals and day treatment programs. I just wanted to acknowledge your experience with your state psychological association pushing political ideologies. During covid, I was surprised that neither my state psychological association or the American Psychological Association came out with any type of public statement saying that school closures were detrimental to the mental health of children. Psychological research clearly had shown how important regular socialization with peers is for children’s mental health. I thought this kind of a public statement could be made with the caveat that the association was not advising whether or not keeping schools closed would affect the transmission of covid. I brought my concerns to the state psychological association via their email listserv, where I was attacked by psychologists who were petrified of covid spreading if schools were to reopen.
Two local psychological associations I’ve been a part of have promoted the narrative of affirming gender dysphoria by offering continuing education for presentations where this was taught with no opposing viewpoints offered.
The American Psychological Association recently came out with a pro-gender affirming “policy statement.” https://www.apa.org/about/policy/transgender-nonbinary-inclusive-care.pdf.
There is an organization called “Therapy First” https://www.therapyfirst.org that supports a “gender exploratory” rather than an automatically affirming model of care, which I support.
I really hope someone sees this. I’m a disabled veteran, a single mother, and I graduated with my BS in Texas. This is a two part problem, one as a veteran and another that I don’t see being discussed: mental health in the workplace.
I had to quit my job with the state because they absolutely refused to accommodate me. Despite the agency having their own policy to support the request, HRs denial having anything to do with hardship relative to what is defined in the CFR, and even though I had two doctors: my primary and specialist request on my behalf for accommodations and provided the necessary paperwork.
I could not find a single lawyer to help me unless I ended up being fired, or was completely denied accommodations, which took the agency 9 months to determine after i submitted my accommodations request. I was able to get one consultation who recommended I submit to the agencies lawyers a discrimination complaint. After doing so, the retaliation began.
There were MANY missteps conducted by a single HR
representative that the agency has to oversee ALL disability requests, including being ignored entirely and missing the point of the interactive process. The most egregious incident was in the denial email from HR my doctors were partially quoted and that information was among managers in my section. This is protected health information that they shared.
Additionally, my issue is with my doctor within the VA who did not seem to care whatsoever despite having a long relationship with her and having gone to her for multiple MH issues.
My main issues with the unfolding of these events and the things I learned along the way:
- FIX THE STATES STATUE OF LIMITATIONS by making it illegal to have them in the first place. How do you put a time limit on a person with a disability to advocate for themselves? This is the equivalent to putting a timed meter on handicap parking. Are we not aware that people with disabilities have medical issues to manage and that TIME is not our friend?
- FIX THE CFR stop giving business’s and corporations the power to interpret and argue the regulations with vague and broad clauses. For example, an accommodations request made by a qualified individual should be resolved expeditiously- GIVE THEM A TIME LIMIT of 30 days to determine.
- VETERANS who are referred outside of the VA to obtain treatment or diagnoses should be REFLECTED WITH SAID DIAGNOSES within the VA system, IMMEDIATELY. There is a major disconnect between what my VA doctor has in my medical records versus what my medical records at multiple specialists in town have. FOR WHAT REASON? I was denied further help for employment because my medical record at the VA does not reflect the worsening of my disabilities.
- ELIMINATE THE STIGMA WITHIN THE VA that unless you went to war, got blown up, shot, etc., you are not a priority. The dick measuring contest is over and the federal government is forking out the money. THE LEAST they could do is take your care seriously.
I skimmed through this but looks like alot of great ideas! We desperately need better mental health resources , I have had family with severe mental health disorders who have state medicaid and wait months for care and then get terrible care when they do get it bc therapists who accept medicaid are swamped!
I would add something I think of importance which is to add some regulation around sites like betterhelp , where the therapists are paid or incentivized to keep clients for long periods and/or volume of clients, instead of improving their outcomes and giving them the best care.
I’m a psychologist in private practice and have been a psychologist for about 30 years. I take insurance in my practice, so I am considered “in network” with several companies. One of the problems I see is that a therapist gets paid the same amount by an insurance company no matter how severe the problem is in the person they are treating. The diagnosis given to the person does not matter. In other words, the therapist gets paid the same amount for “individual psychotherapy” no matter if the person is suicidal or if they are depressed over a recent life event. They also get paid less for “couples counseling” than they do for individual therapy, even though it is more difficult to do. Usually people with the most severe problems tend to go to agencies (like local mental health centers) rather than therapists in private practice, because they don’t have private health insurance. Agencies typically provide little psychotherapy and rely much more on psychiatric medication, which tends to be over prescribed and has lots of negative effects. Agencies are also usually staffed by therapists with the least experience, because therapists want to go into private practice where they have more autonomy and typically see patients with less severe problems. So unfortunately, those with the most difficult to treat problems end up with therapists (if they are so lucky) with the least amount of experience and training.
I worked at a state psychiatric hospital for a year as an intern. It was heartbreaking that almost no one there had EVER had an individual therapist to talk to about their life or traumas they had experienced. To me, what I saw was about “control and management” of people, not healing or helping them. If someone was in distress and causing a disturbance, the first thing that would happen was that they’d be give a PRN (as needed) medication. If that didn’t work, they’d be locked in a room. If that didn’t work, there would be a “take down” where the person would be forcibly put into 5 point restraint and injected with more drugs to knock them out.
Just like in any profession, there are some therapists who are good at what they do and others not so much so. Therapy is an art as well as a science. One needs the ability to connect with and empathize with others, be doing their own personal healing work, and receive quality training and supervision. Unfortunately, because of the need for more mental health professionals, it seems there has been a proliferation of programs that are online or of lesser quality. This isn’t to say that doctoral or in person programs produce more effective therapists than do less time intensive programs, but in general, the more experience and more clinical supervision one has, the more equipped one is to be an effective therapist. I’ve also found there is a wide variety in the quality of continuing education programs that are approved for ongoing training. Some are absolutely useless and others provide ongoing training in psychotherapeutic techniques at an advanced level, where one is videotaping client sessions for supervision, which is one of the best ways to learn to be a better therapist.